Could funding disparities be weakening the capacity of cancer research to improve patient lives? Yes, according to the findings published in a Lancet paper, Global funding for cancer research between 2016 and 2020: a content analysis of public and philanthropic investments.
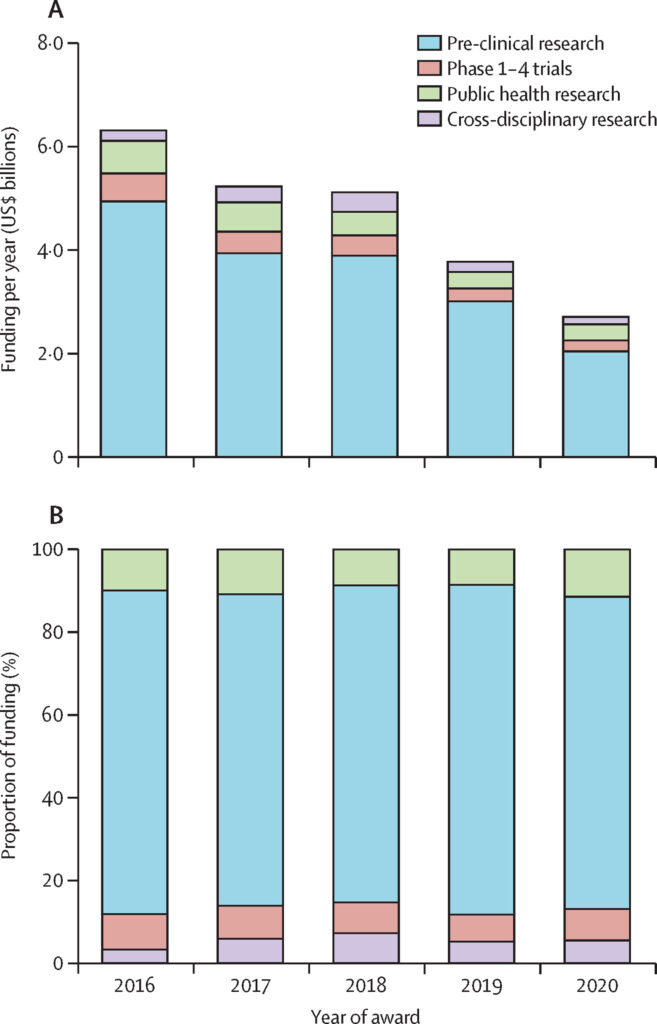
A new study has shown major disparities between research funding for cancer treatments and how they are implemented. On analyzing funding flows from public and philanthropic awards for cancer research, the authors of the recent Lancet paper found multiple levels of disconnect between ground reality and the funding flows. The findings were based on the content analysis of research award data from 2016 to 2020 mined from the Dimensions database. According to the authors the study is the “first comprehensive global analysis of cancer research funding, covering about $24·5 billion of global investment, from 66,388 public and philanthropic awards.”
But why is it crucial for multiple stakeholders in healthcare to have clear insights into the disparities in the current cancer research funding? Because the global burden of cancer, which was 19 million cases in 2020, is expected to grow to 28 million by 2040. And, according to the World Health Organization, cancer continues to be a leading cause of death worldwide; it accounted for nearly 10 million deaths in 2020, that is, nearly one in six deaths globally.
Underfunding of cancers with high burden
One disconnect highlighted in the study was the level of funding given to research on different types of cancers. To contextualize their findings,the authors used a measure “years lived with disability”, which considers the effect of that disease on quality of life, and they also looked at what investment 18 different types of cancer received and compared this against the number of deaths caused annually by each type of cancer. They found that thyroid cancer and lung cancer were the least well-funded considering their global health burdens. In particular, they found that lung cancer research was poorly-funded considering the high death rate associated with the disease. And, while the research investment of 2.73 billion USD (11.2% of the funding) on breast cancer, appeared proportionate to the disease burden (11·7% of cases and 6·9% of deaths), research focusing on lung cancer, which accounted for 11·4% of cases and 18% of deaths globally, received only 5·3% of the investment. Conversely, data showed that although relatively uncommon, brain cancers received the highest investment per burden metric.
Preclinical research and immuno-oncology get a sizable chunk of funding. But should they?
The authors also looked at which stages of research and types of treatment research command the most funding. Their findings show that preclinical investigations, typically carried out in controlled laboratory settings, received a whopping 18 billion USD (73.5%) in funding. The problem: it can take up to 17 years for preclinical investigations to make it to real-world settings. And there is evidence showing that prevention and early detection are key to cancer control globally. “However, despite this, our analysis reveals that only a relatively small proportion of research investment is directed at cancer detection and diagnosis,” the authors write.
On looking at the funding flows into research on treatment approaches, the team found that surgery and radiotherapy, the mainstay treatments for most solid tumors, were underfunded as compared to drug treatment research and immuno-oncology. In 2015, it was estimated that over 80% of new cancer cases needed surgery, and about 50% needed radiotherapy. But, the data on research funding showed that only a small percentage, about 1.4%, goes to surgical research and 2.8% is directed toward radiotherapy research. On the other hand, drug treatment research gets the lion’s share, around 20%, even before it reaches the clinical trial stages, and the fast-growing area of immuno-oncology gets 12.1% of the funding.
Unmet funding needs of low- and middle-income countries (LICs)
The authors write that the (above-mentioned) narrow funding focus on preclinical research and on novel areas such as immuno-oncology directly feeds into global health inequalities. Even if immuno-oncology and other innovative therapies find their way into clinical application, these breakthroughs will be predominantly accessible in wealthier nations, with the underprivileged populations unlikely to have access to the most recent treatment options. Moreover, a mere 0.5% of cancer research funding was directed towards LICs, making it challenging for people in less affluent countries to reap the benefits of novel research discoveries.
The study also revealed an average annual expenditure on cancer research from 2016 to 2019 amounting to US$5.5 billion per year plummeted by 45% to US$2.9 billion in 2020, likely due to the focus on the COVID-19 pandemic. The authors anticipate that the reductions in funding will result in a reduced flow of new knowledge within the cancer research domain and compound the challenges faced by patients in LICs precisely when the global cancer burden is expected to rise, potentially intensifying disparities in access to cancer treatment and care.
“Any funding redistribution will require joint research priority setting across multidisciplinary stakeholders, including patients, to ensure that research is addressing key issues of concern to the cancer community. There are finite resources available for research and development investment across cancer and health. We must invest wisely,” the authors conclude.