Even before the pandemic, the human and economic cost of infectious diseases was jaw-dropping. In 2020 a research paper* put the economic burden of eight major diseases (HIV/AIDS, malaria, measles, hepatitis, dengue fever, rabies, tuberculosis and yellow fever) at up to US$8 trillion. And over 156 million life years were lost in 2016 alone.
A major new analysis from Nature Index has tracked over 80 infectious diseases for 20 years, drawing heavily on Digital Science’s Dimensions database as well as its own. Nature Index Infectious Disease – published as a supplement to Nature – monitors the economic cost and human impact of these diseases. It also examines the research output on each, shining a light on the research – and the people and institutions behind it – that aims to reduce this high burden.
The Nature Index is a database of author affiliations and institutional relationships. It tracks contributions to research articles published in 82 high-profile scientific journals, chosen by an independent panel of researchers from different fields.
What sets this new study apart is its unusually extensive scope and timeframe. It covers 83 diseases, from anthrax to Zika, over a 20-year period. Using a separate set of keywords for each disease plus 5 subcategories (for coronavirus and influenza), the Nature Index team carried out keyword searches of abstracts and titles in the Dimensions database. This produced nearly 1.7 million articles for 2000-2020, including 9,816 for 2015-2020 that are also tracked in the Nature Index database.
Dimensions produces maximum insight and accuracy by allowing the user to enter highly complex search strings. For example, the search string used for Covid-19 was “COVID-19” OR “2019-nCoV” OR “SARS-CoV-2” OR “HCoV-2019” OR “NCOVID-19” OR “severe acute respiratory syndrome coronavirus 2” OR “severe acute respiratory syndrome corona virus 2” OR “coronavirus disease 2019”.
Two main findings
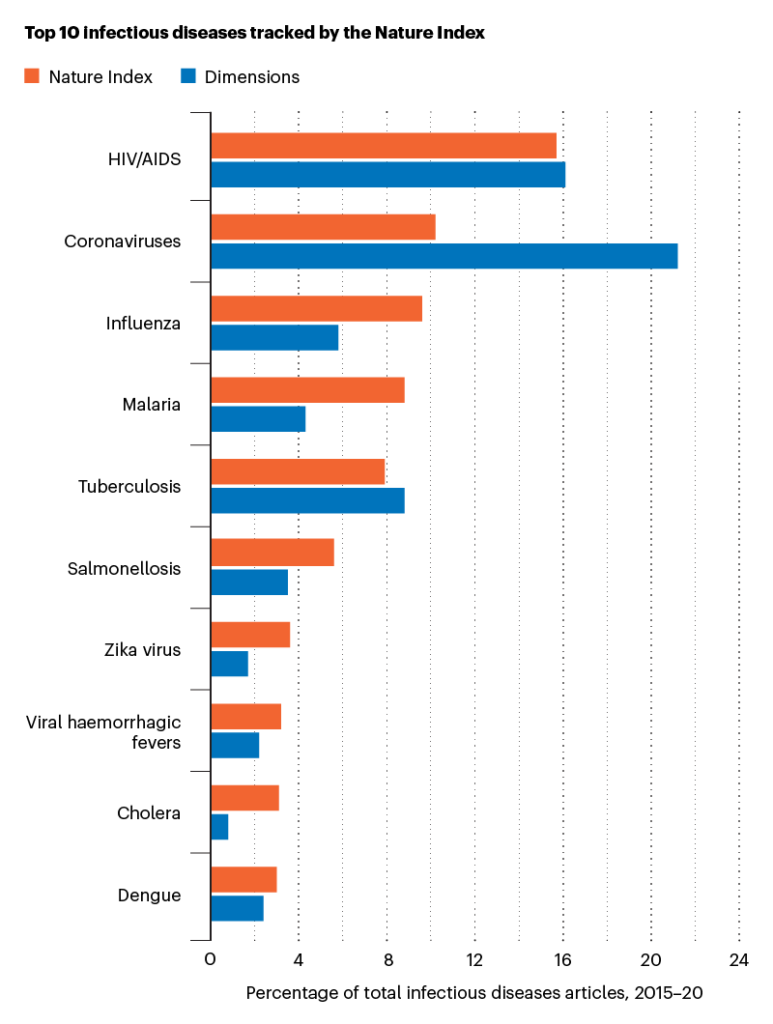
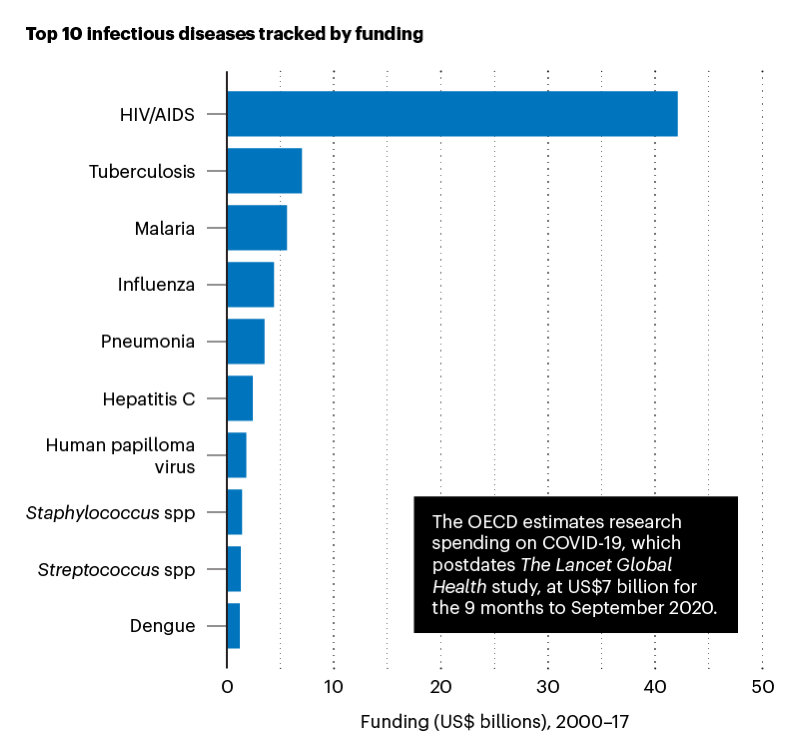
Two key themes stand out. First, several of the world’s deadliest diseases receive less research attention and research funding than others with less health impact.
For example, tuberculosis is the second deadliest infectious disease, killing 1.5 million people in 2020, despite being preventable and curable. However, in 2000-2017 HIV/AIDS received six times more funding than tuberculosis.
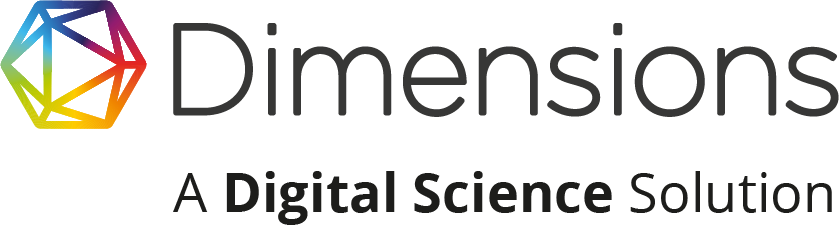
In the Nature Index, articles related to HIV account for 15.7% of infectious disease-related articles for 2015–20, the highest of any infectious disease. In the Dimensions database, coronavirus dominates with 21.2% of infectious diseases articles. And the vast majority of these articles are related to COVID-19, accounting for 19.7% of infectious disease-related articles in Dimensions for 2015–20.
Top infectious diseases in Dimensions that do not appear in the Nature Index top 10 are human papillomavirus (ranked fourth), hepatitis C (ranked sixth) and hepatitis B (ranked 8th).
A second key theme is that progress will need new collaborative, multi-sectoral and transdisciplinary approaches. One example highlighted in the study is the Pfizer-BioNTech collaboration that produced the highly effective COVID-19 mRNA vaccine. Another is the Tuberculosis Drug Accelerator (TBDA), a multidisciplinary consortium of pharmaceutical companies and academic scientists. Launched in 2012 with support from the Bill and Melinda Gates Foundation, it aims to speed up the discovery and development of new drugs to treat TB.
Other notable findings
Leading countries
Looking at the leaders in the fight against infectious disease, the study finds that the US dominates infectious diseases research output in the Nature Index, with nearly five times the share of China in second place. By contrast, Japan is surprisingly low down the list.
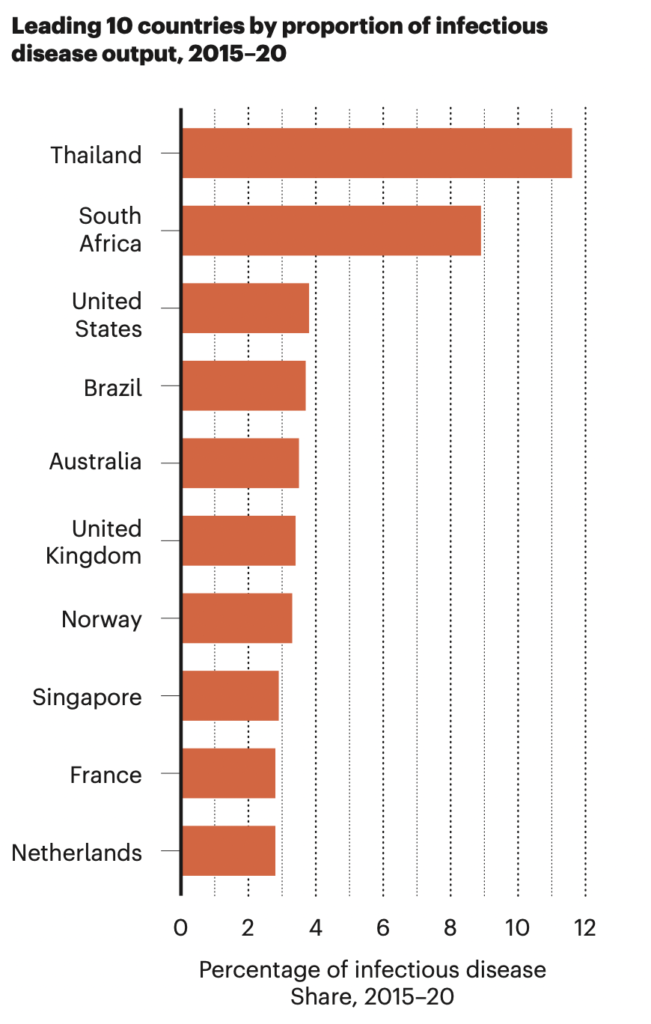
Among the leading 25 countries for infectious diseases output, Thailand and South Africa have the highest proportion of output related to the topic. But compared with countries like the US and the UK, their total share is low.
Rising resistance
After a decade of slow growth in the early 2000s, research into antibiotic resistance has shot up. The Dimensions database has seen a dramatic rise in output of articles on this topic, growing by 150.9% between 2015 and 2020, and by 24% in 2019-20. The Nature Index saw even faster growth of 165.3% between 2015 and 2020.
An ongoing challenge
COVID-19 has made it more urgent than ever to confront the societal and scientific challenges that spring from infectious disease. This study underlines the vital role of research in helping us overcome these challenges – and the vital role of data in steering that research in the right direction.
Footnote
*Modern Infectious Diseases: Macroeconomic Impacts and Policy Responses, Institute of Labour Economics, August 2020
Sign up for news and updates from Dimensions